


Evolving Enzymes
Inovating IVD




Cancer immunologists scoop medicine Nobel prize

James Allison and Tasuku Honjo share the 2018 Nobel Prize in Physiology or Medicine. Left: Richard Drew/AP/Shutterstock. Right: MEXT/CC BY 4.0
Two scientists who pioneered an entirely new way to treat cancer have won the 2018 Nobel Prize in Physiology or Medicine.
James Allison at the University of Texas MD Anderson Cancer Center in Houston and Tasuku Honjo at Kyoto University in Japan will share the 9 million Swedish kronor (US$1 million) prize.
The pair showed how proteins on immune cells can be used to manipulate the immune system so that it attacks cancer cells. The approach has since led to the development of therapies that have been hailed for extending survival in some people with cancer by years, and even wiped out all signs of disease in some people with advanced cancers. Researchers have flocked to the approach, and immunotherapy is now one of the hottest areas in cancer research.
Early excitement
Allison is in New York for an immunology conference, and was awoken at 5.30 by a call from his son delivering the good news. By 6.30, colleagues were banging on the door of his hotel room bearing champagne for an impromptu party. The Nobel Committee only reached him some time after that.
“It still hasn’t completely dawned on me,” said Allison, at a press conference. “I was a basic scientist. To have my work really impact people is one of the best things I could think about. It’s everybody’s dream.”
In the 1990s, Allison, then at the University of California, Berkeley, was one of several scientists who studied a ‘checkpoint’ protein, CTLA-4, that acts as a brake on immune cells called T cells. In 1997, Allison and his colleagues engineered an antibody that could bind to CTLA-4, removing the brakes on T-cell activity and unleashing them to attack cancer cells in mice. A clinical study in 2010 found that the antibody had a striking effect on people with advanced melanoma, a form of skin cancer1.
Working independently of Allison, in 1992, Honjo discovered a different T-cell protein, PD-1, which also acts as a brake on the immune system but by a different mechanism. PD-1 went on to become a target in the treatment of cancer. In 2012, research in people revealed that the protein was effective against several different cancers, including lung cancer, a major killer2. The results were dramatic — some patients with metastatic cancer went into long-term remission, raising the possibility of a cure.
Releasing the brakes
“Allison’s and Honjo’s discoveries have added a new pillar in cancer therapy. It represents a completely new principle, because unlike previous strategies, it is not based on targeting the cancer cells, but rather the brakes — the checkpoints — of the host immune system”, said Klas Kärre, a member of the Nobel Committee and an immunologist at the Karolinska Institute in Stockholm who described the work of the prizewinners during the Nobel announcement. “The seminal discoveries by the two laureates constitutes a paradigmatic shift and a landmark in the fight against cancer.”
In recent years, clinical work on drugs that inhibit the CTLA-4 and PD-1 mechanisms — known as ‘immune checkpoint therapy’ — has developed apace. Treatments that block PD-1 have been shown to be effective in lung and renal cancers, lymphomas and melanoma. Recent clinical work that combined therapies targeting CTLA-4 and PD-1 in patients with melanoma showed that this approach can be even more effective than CTLA-4 alone3. Trials are now underway to evaluate the efficacy of checkpoint therapy against most types of cancer, and scientists are testing numerous other checkpoint proteins to see if they could act as targets.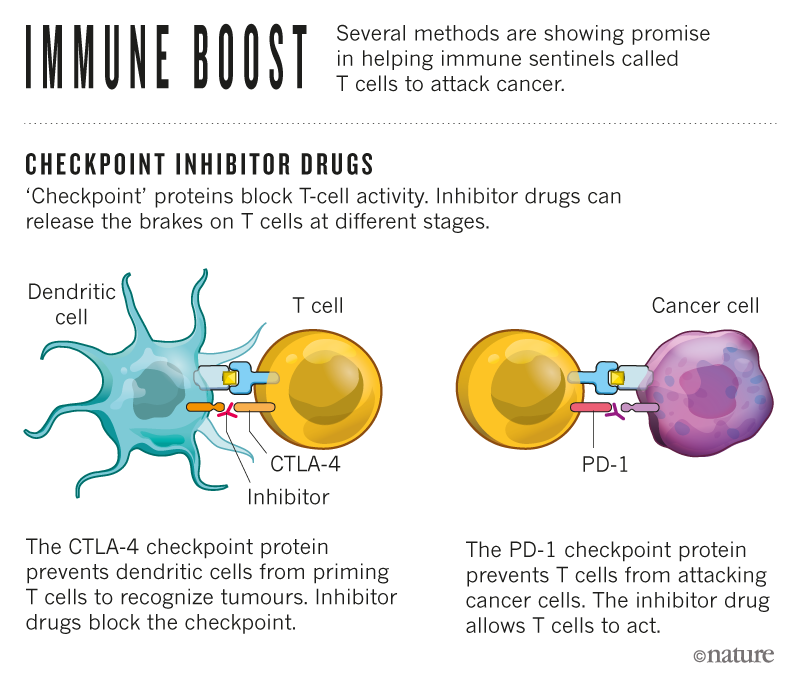
But Allison and Honjo were not alone: others also made important early discoveries about checkpoint inhibitors, notes Gordon Freeman, an immunologist at the Dana-Farber Cancer Institute in Boston, Massachusetts, who was disappointed not to be recognized for his contributions. Freeman, along with immunologists Arlene Sharpe at Harvard Medical School in Boston and Lieping Chen at Yale University in New Haven, Connecticut, studied PD-1 and a molecule that binds to it called PD-L1.
The drug ipilimumab, an antibody that inhibits CTLA-4, won approval from the US Food and Drug Administration (FDA) in 2011 and was the first checkpoint inhibitor to reach patients. But Freeman points out that CTLA-4 inhibitors have so far been shown to work only in melanoma. And the FDA has approved drugs that target PD-1 and PD-L1 to treat 13 different cancers. “PD-1 and PD-L1 are what works in a really wide variety of people,” he says. “And our discoveries were foundational there.”
However, Freeman says that CTLA-4 paved the way, and that Allison had a key role in pushing the field. “Jim Allison has been a real advocate and champion of the idea of immunotherapy,” he says. “And CTLA-4 was a first success.”
Obvious choices
Immunologist Jerome Galon of the French national biomedical research agency, INSERM, in Paris, was not surprised by the committee’s decision to award the prize to Honjo and Allison. “I think they really deserve it,” he says. “You can always multiply and have many other people, but these are the obvious two first choices.”
He adds that the prize reflects how far the immune approach to fighting cancer has come. When PD-1 inhibitors were shown to work against lung cancer in 2012, the field ignited, with researchers in academia and industry racing to find ways to expand the number of patients who could benefit from the drugs. “Ten years back, nobody was interested — nobody except a few immunologists,” Galon says. “It’s such a big change.”
In a 2013 interview with Nature, Allison described the resistance he met when he first tried to get pharmaceutical companies interested. “It was very frustrating,” he said. “They said, ‘It may work in mice, but it’ll never work in people’. The concept was new and it was so unusual.”
Allison marched from company to company in search of one that would take on the project. Ultimately, Bristol-Myers Squibb of New York City was the one to push ipilimumab over the finishing line. Since then, other pharmaceutical companies have developed checkpoint inhibitors that have been approved for use in people.
Combination therapy
A major draw, says Galon, is the potential of these drugs to lengthen patients’ lives by years, rather than just weeks or months. But only a fraction of patients experiences such dramatic responses, and researchers are racing to boost those numbers by combining checkpoint inhibitors with each other and with other treatments. “The huge benefit in comparison to other treatments is that patients are experiencing long-term survival,” he says. “Unfortunately, only a subgroup of patients is responding.”
Through it all, it’s been thrilling to watch the field develop, says Freeman. “It’s really been just an incredible amount of human creativity and energy,” he says. “It’s wonderful because so many cancer patients are doing better.”
In 2015, Allison won a prestigious Lasker prize for his work on cancer immunotherapy. In 2016, Honjo won the Kyoto Prize in basic sciences, a global prize awarded by the Inamori Foundation.






